Hypothermia in preterm infants
- Introduction...
- 1. Learning object...
- 2. Effect of hypot...
- 3. Effect of low a...
- 4. Admission tempe...
- 5. Effect on incid...
- 6. Thermoneutral z...
- 7. Mechanisms of h...
- 8. Heat loss by co...
- 9. Heat loss by co...
- 10. Heat loss by c...
- 11. Heat loss by r...
- 12. Heat loss by e...
- 13. Risk factors...
- 14. Brown fat...
- 15. Body surface a...
- 16. Skin changes...
- 17. Preterm prone ...
- 18. Key messages...
 |
 |
Introduction
DR. TEJO PRATAP OLETI
MD, DM (Neonatology)
Consultant
Department of Neonatology
Fernandez Hospital
Hyderabad
1. Learning objectives
► Effect of hypothermia on mortality and morbidities
► Thermal well being in preterm infants
2. Effect of hypothermia

3. Effect of low admission temperatures
► For each drop in 1°C
♦ Mortality – increases by 28%
♦ Late onset sepsis – 11%
* Laptook et al. Pediatrics; 2007
4. Admission temperatures – mortality/ morbidities


* Lyu et al. JAMAP Pediatrics 2015
5. Effect on incidence of mortality and morbidity
► Interventions to prevent hypothermia will lead to decrease
in mortality and morbidities by 18% – 42%
* UNICEF. Progress for children: a world fit for children
statistical review. New York, NY: United
Nations Children`s Fund; 2007
6. Thermoneutral zone (TNZ)

7. Mechanisms of heat transfer
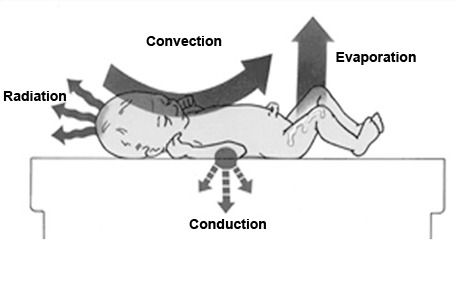
8. Heat loss by convection
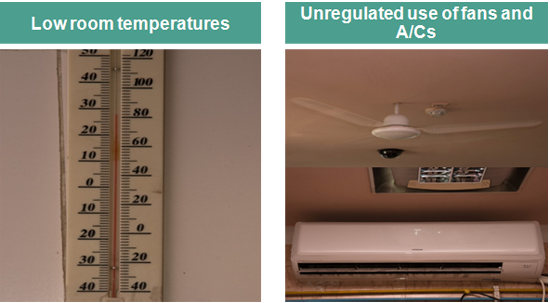
9. Heat loss by convection
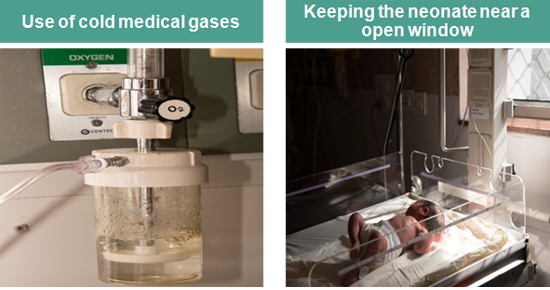
10. Heat loss by conduction

11. Heat loss by radiation
► Nursing the neonate near a cold wall
► Inadequate clothing
► Too many cold objects in the room
12. Heat loss by evaporation
► Delayed drying at birth
► Prolonged contact with wet linen
► Frequent bathing
► Wet diapers

13. Risk factors
Why preterm are at higher risk?
► Lesser brown fat tissue
► Larger surface area per unit kg weight
► Skin immaturity
► High transepidermal water loss
14. Brown fat
► Contributes to 4-10% of fat tissue
► Main source of non-shivering thermogenesis
► Not detectable before 26-30 weeks of gestation
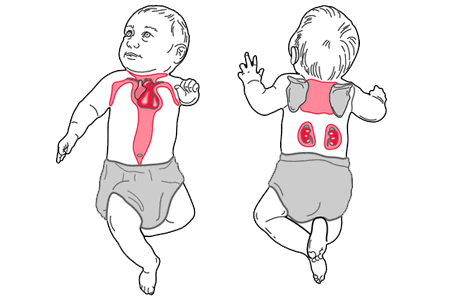
15. Body surface area

► 7 times more per unit (kg) weight compared to adults
extended posture will expose more body surface area
16. Skin changes
► 20 to 30% thinner than the adult skin
► More thinner epidermis
► Less hydrated and has reduced natural moisturization
factors
► Increased insensible loss of water

17. Preterm prone for injuries
► Increased insensible loss of water


18. Key messages
► Hypothermia: increased mortality and major morbidities
► Ideal environmental temperature is based on
♦ Weight
♦ Day of life
♦ Clothing
♦ Sickness
► Thin stratum corneum, increased IWL, larger body
surface area and lesser brown fat: risk factors
