Management of jaundice in preterm neonates
- Introduction...
- 1. Total serum bil...
- 2. Important consi...
- 3. Important consi...
- 4. Management of a...
 |
 |
Introduction
Dr. C. APARNA
MD, DM (Neonatology)
Consultant Neonatologist
Ankura Hospital for Women and Children
Kukatpally, Hyderabad
1. Total serum bilirubin thresholds for treatment of jaundice in preterm neonates
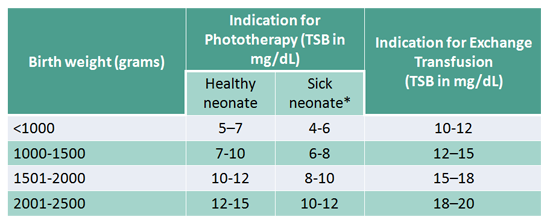
SICK NEONATE DEFINED AS:
♦ Rapidly rising TSB levels (>0.5 mg/dL/h), suggesting
hemolysis
♦ Neonates with clinical instability/sepsis/ asphyxia
2. Important considerations while managing a preterm neonate with jaundice
► Neonates with any of the following conditions in the
previous 24 hours are considered to have clinical instability
a) Apnea requiring bag and mask ventilation
b) Hypotension requiring pressors and
c) Mechanical ventilation at the time of blood sampling
► Use total serum bilirubin; Do not subtract the direct fraction
unless > 50% of the total
► Use lower value of the range presented in neonates of lower
birth weight/ gestational age
3. Important considerations to decide need for exchange transfusion
► Exchange transfusion (ET) is recommended if the TSB
exceeds the threshold for exchange transfusion or if the
neonate shows signs of suspected acute bilirubin
encephalopathy (signs can be non-specific in preterm
neonates) irrespective of the level
► Recommendations apply to neonates who are receiving
intensive double surface phototherapy to the maximal surface
area but whose TSB levels continue to increase
► Start intensive PT pending arrangement for ET
► Repeat total serum bilirubin
♦ Q12-24 hourly
♦ More frequently, if there is a setting for hemolysis
4. Management of a neonate receiving phototherapy
► No role for clinical assessment or TcB while under
phototherapy
► Repeat total serum bilirubin
♦ Q12-24 hourly
♦ More frequently if there is a setting for hemolysis
► Discontinue phototherapy when TSB is 2 mg/ dL below the
threshold for phototherapy
