Antibiotic therapy for sepsis in neonates
- Introduction...
- 1. Learning object...
- 2. Harms of excess...
- 3. Initial choice ...
- 4. When to upgrade...
- 5. Changes after c...
- 6. How long to giv...
- 7. How to reduce t...
- 8. No antibiotics...
- 9. Best practices...
- 10. Take home mess...
 |
 |
Introduction
DR. S. VENKATASESHAN
MD, DM (Neonatology)
Associate Professor
Department of Pediatrics
PGIMER, Chandigarh
1. Learning objectives
► Why rational use of antibiotics?
► Initial choice?
► When to upgrade?
► How long to give?
► Best practices?
2. Harms of excessive use of antibiotics
► High risk of antibiotic resistance
► Higher risk
♦ Invasive candidiasis
♦ NEC
♦ Death
3. Initial choice of antibiotics
► Should cover both gram + ve and – ve bacteria
► Suggested plan
1. Community acquired
♦ Ampicillin + aminoglycoside
♦ Evidence of Staphylococcus infection: cloxacillin in place
of ampicillin
2. Hospital acquired
♦ (Cloxacillin or ampicillin)* + aminoglycoside
► Avoid third generation cephalosporins/ carbapenem/
vancomycin
*Choice between cloxacillin and ampicillin depends on the prevalent flora in the unit
4. When to upgrade?
► Worsening or absence of improvement after 48 hours
► Early escalation may be considered if baby becomes
extremely sick or deteriorates rapidly
► Second line antibiotics based on
1. Culture report (if available)
2. Unit policy (sensitivity pattern)
5. Changes after culture report
► Sensitive to an antibiotic with narrower spectrum
♦ Change even if the neonate was improving
► Use only one antibiotic to which organism is sensitive
6. How long to give?
► Use parenteral antibiotics
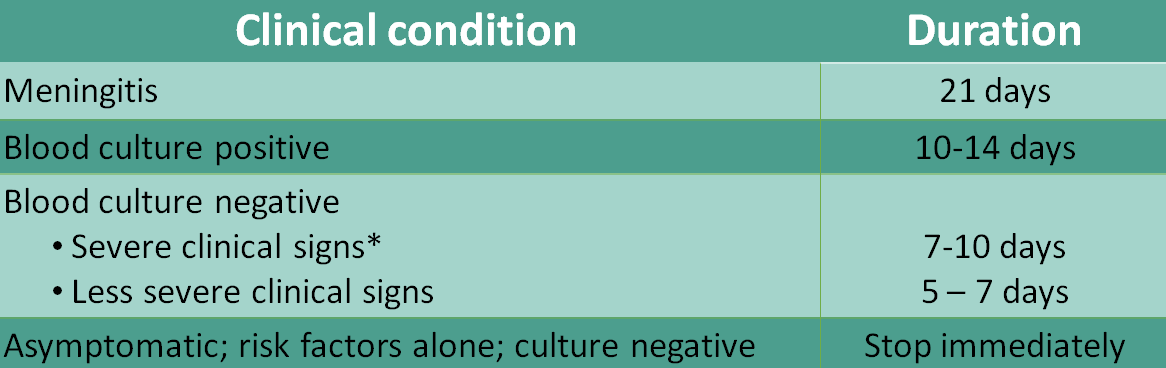
*Shock, sclerema, DIC, severe hypothermia, seizures
7. How to reduce the duration?
► Collect blood culture reports on time
♦ Phone/ online/ SMS
► Trust your lab
♦ Blood culture positivity rates: 15-35%
► Get the culture report faster - use BACTEC or other automated
blood culture systems
8. No antibiotics
► Non-infectious conditions such as
♦ Asphyxia
♦ Meconium aspiration
♦ Prematurity/ low birth weight
► Procedures such as
♦ Exchange transfusion
♦ Central line/ umbilical line insertion
♦ Intubation
♦ Phototherapy
9. Best practices
► Have a written antibiotic policy and follow it
♦ When, which, how & how long
♦ Track organism profile
► Do not give antibiotics
♦ As prophylaxis
♦ Parenteral route for superficial skin infection
► Establish correct diagnosis
♦ Send blood culture before starting antibiotics
► Prescribe right dose using drug formulary
10. Take home messages
► Have a written antibiotic policy for your unit
► Send blood culture before starting antibiotics
► Based on culture and clinical signs, stop antibiotics at the
earliest
► Document indication, review date and proposed duration
► Follow right dose and frequency
► Follow instructions for drug administration
