Care of babies after discharge from NICU
- Introduction...
- 1. Care of preterm...
- 2. Learning object...
- 3. Discharge plann...
- 4. Discharge summa...
- 5. Discharge plann...
- 6. Growth targets...
- 7. Preterm growth ...
- 8. Fetal-infant Gr...
- 11. Complementary ...
- 12. Immunization -...
- 13. Birth doses of...
- 14. Education of p...
- 15. Screening of p...
- 16. ROP screening...
- 17. Eye checkup at...
- 18. Hearing screen...
- 19. Neurodevelopme...
- 20. Opportunity to...
- 21. Intact outcome...
- 22. Table 01...
- 23. Table 02...
- 10. WHO growth cha...
- 9. Fetal-infant Gr...
 |
 |
Introduction
DR. NAVEEN JAIN
MD, DM (Neonatology)
Senior Consultant
Department of Pediatrics
Kerala Institute of Medical Sciences
Trivandrum
1. Care of preterm infants after hospital discharge
► Some of the preterm babies are at risk of neurodisability
► Screening of these at - risk babies, timely referral &
intervention will decrease disabilities
2. Learning objectives
Comprehensive care of preterm babies after discharge from the hospital
► Discharge planning
► Medical care
♦ Growth monitoring
♦ Recommendations on nutrition after discharge
♦ Recommendations on vaccination
► Neurodevelopment assessment
♦ Recommendations on screening (for prevention of
neurodevelopment disability, NDD)
♦ Suggested follow up schedule for assessment
with development
3. Discharge planning
► Each unit should have place dedicated to follow up services
that include all/ most of the services under one roof
► Dedicated personnel must coordinate the screening of at-risk
babies
► The unit may plan one or more days of the week dedicated
to follow up
4. Discharge summary
► The discharge summary must include baby’s gestation,
birth weight and risk factors for neurodevelopment – e.g.
♦ Antenatal steroids given/ evidence of fetal growth
restriction/ fetal distress/ chorioamnionitis
♦ Need for resuscitation at birth
♦ Need for oxygen/ ventilation
♦ Shock/ need for blood transfusion
♦ Sepsis/ meningitis
♦ Adequacy of growth
♦ Hypoglycemia/ jaundice
5. Discharge planning – checklist
► Medical care
♦ Weight tracking on preterm growth chart
♦ Head circumference tracking
♦ Nutrition advice
♦ Immunization advice
► Neurodevelopment assessment
♦ ROP screening done/ scheduled
♦ Vision evaluation educated
♦ Hearing screen done/ scheduled
♦ Neuro sonogram done/ scheduled
♦ KMC
♦ Parent readiness for discharge
6. Growth targets
► Once preterm babies regain their birth weight (BW),
expected growth targets are:
♦ Weight – 15 to 20 gm/ kg per day
♦ Head circumference – 0.5 to 1 cm /week
♦ Length – 1 cm/week till 40 weeks
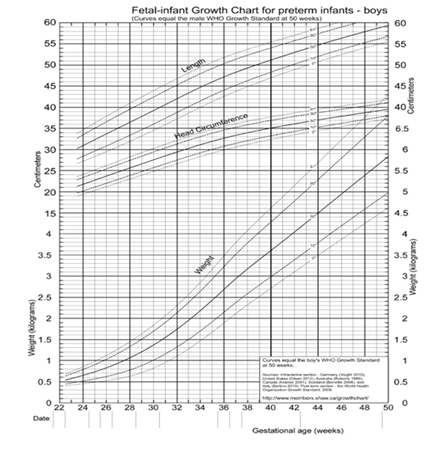
7. Preterm growth charts
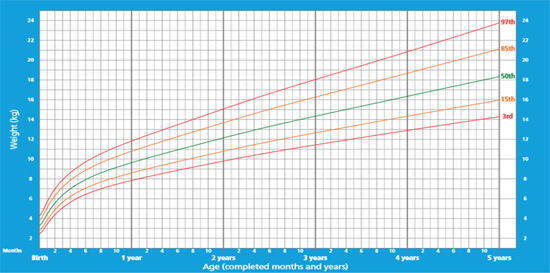
► Weight, length and head circumference should be measured
even when baby is in NICU and continued after discharge
► 1-2 weekly (after discharge from hospital) for a few weeks,
then at each health care visit for vaccination
► The growth parameters must be plotted and growth
tracked on growth charts for preterm babies (example:
Fentons growth chart)
8. Fetal-infant Growth Chart for preterm infants - GIRLS

11. Complementary feeding
► Exclusive breast milk must be continued till 6 months
of age corrected for prematurity
► Complementary feeding with semisolid foods should be
started at 6 months of age
► There is no change in age of starting complementary
feeding for preterm babies
12. Immunization - no change for preterm babies
► The immunization schedule remains unchanged for preterm
babies (chronological age: counted from the date the baby
was born)
► Medically stable PT and low birth weight (LBW) infants
should receive full doses of diphtheria, tetanus, acellular
pertussis, Haemophilus influenzae type b, hepatitis B,
poliovirus, and pneumococcal conjugate vaccines at a
chronologic age consistent with the schedule recommended
for full-term infants
13. Birth doses of BCG/ Hep B and OPV at discharge
► The birth doses of BCG, OPV may be given once the preterm
baby is medically stable and ready for discharge (at or after
34 weeks gestation)
► If preterm baby is < 2 kg, one may give Hep B once the baby is
30 days old/ ready for discharge (mother is Hep B negative
or immunized)
14. Education of parents on follow up
Neurodevelopment assessment
► Parents should be educated regarding
♦ The need to test
♦ Follow up schedules
♦ Possible interventions if a deviation from normal
is detected
15. Screening of preterm babies – to prevent NDD
► ROP screening
► Vision assessment at 9-12 months
► Hearing screening and diagnostic tests before 6 months
of age
► Multi - domain development tests at 4, 8 & 12 months
► Neurosonogram at 1-2 weeks and 36- 40 weeks
16. ROP screening
► Often the preterm babies are discharged before the ROP
screening is complete
► The families must be educated on the need to follow up till
ophthalmologist informs that screening is complete/
treatment of ROP is required
17. Eye checkup at 9-12 months
► Preterm babies are at increased risk of strabismus, myopia
and late retinal detachment
► They should undergo examination by an ophthalmologist at
9 to 12 months of age
18. Hearing screen
► Preterm sick babies are at increased risk for sensorineural
hearing loss, so automated auditory brainstem response
(AABR) should be done
► It is best to complete AABR before discharge from hospital
at birth admission
♦ Otoacoustic emissions (OAE) will fail to detect
sensorineural hearing loss
► In baby fails screening tests, confirmation of hearing loss
and intervention must be initiated before 6 months age
19. Neurodevelopment assessment
► Assess neurologic abnormalities (tone)
► Multi-domain development screening
(e.g. CDC grade, Denver II, Bayley screener)
► Time: 4 , 8 and 12 months age corrected for prematurity
► Recognize, refer for early intervention
20. Opportunity to reduce disability
► Appropriate follow up is an opportunity to detect early and
correct deviations in development
► Neonatologist must explain to parents the tests and the
treatments
► Visits to the specialists may be facilitate by dedicated staff
♦ They are involved in parent education, managing
appointments and guiding parents to intervention
programs
21. Intact outcomes
► The goal to save preterm babies without disability can be
achieved by timely screening and appropriate interventions
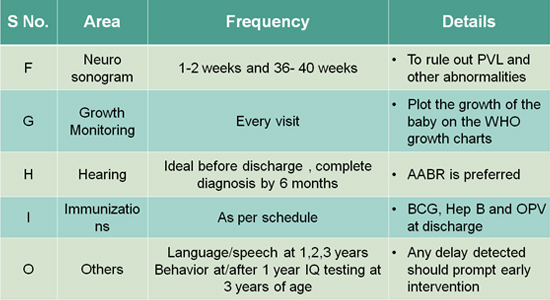
22. Table 01
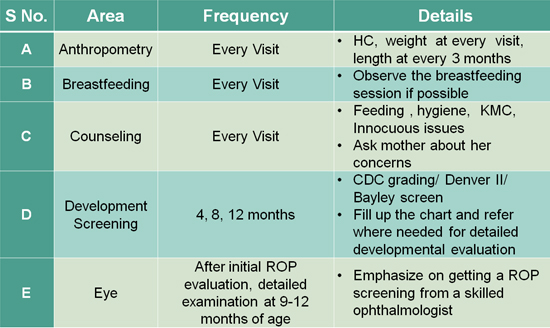
23. Table 02
10. WHO growth chart
9. Fetal-infant Growth Chart for preterm infants - BOYS