Identification of Jaundice in preterm infants
- Introduction...
- 1. Identification ...
- 2. Visual assessme...
- 3. Transcutaneous ...
- 4. Jaundice requir...
 |
 |
Introduction
Dr. C. APARNA
MD, DM (Neonatology)
Consultant Neonatologist
Ankura Hospital for Women and Children
Kukatpally, Hyderabad
1. Identification of jaundice in preterm neonates
► Visual assessment
► Transcutaneous bilirubin (TcB)
► Total serum bilirubin levels (TSB)
2. Visual assessment of jaundice in preterm neonates
► Examine the neonate in bright day light or white light
► Examine blanched skin, sclerae and palate of the neonate
► Assess frequently during every examination of the neonate,
during the first week of life
3. Transcutaneous bilirubin
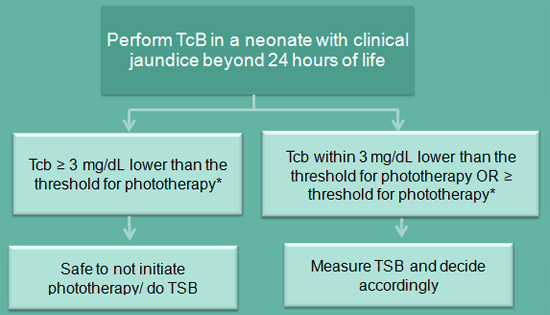
* Age appropriate cut offs for treatment discussed in webinar on treatment of jaundice, TSB- Total serum bilirubin.
4. Jaundice requiring total serum bilirubin (TSB) estimation
► Any visible jaundice in first 24 hours of life
► Beyond 24 hours, TcB levels falling within 3 mg/dl below
OR ≥ the threshold for phototherapy
► Any clinical jaundice in a “sick preterm neonate”*
► During phototherapy and any subsequent measurements
after stopping phototherapy
* Sick preterm neonate defined as :
Rapidly rising TSB levels (>0.5 mg/dL/h), suggesting
hemolysis Neonates with clinical instability/sepsis/ asphyxia
